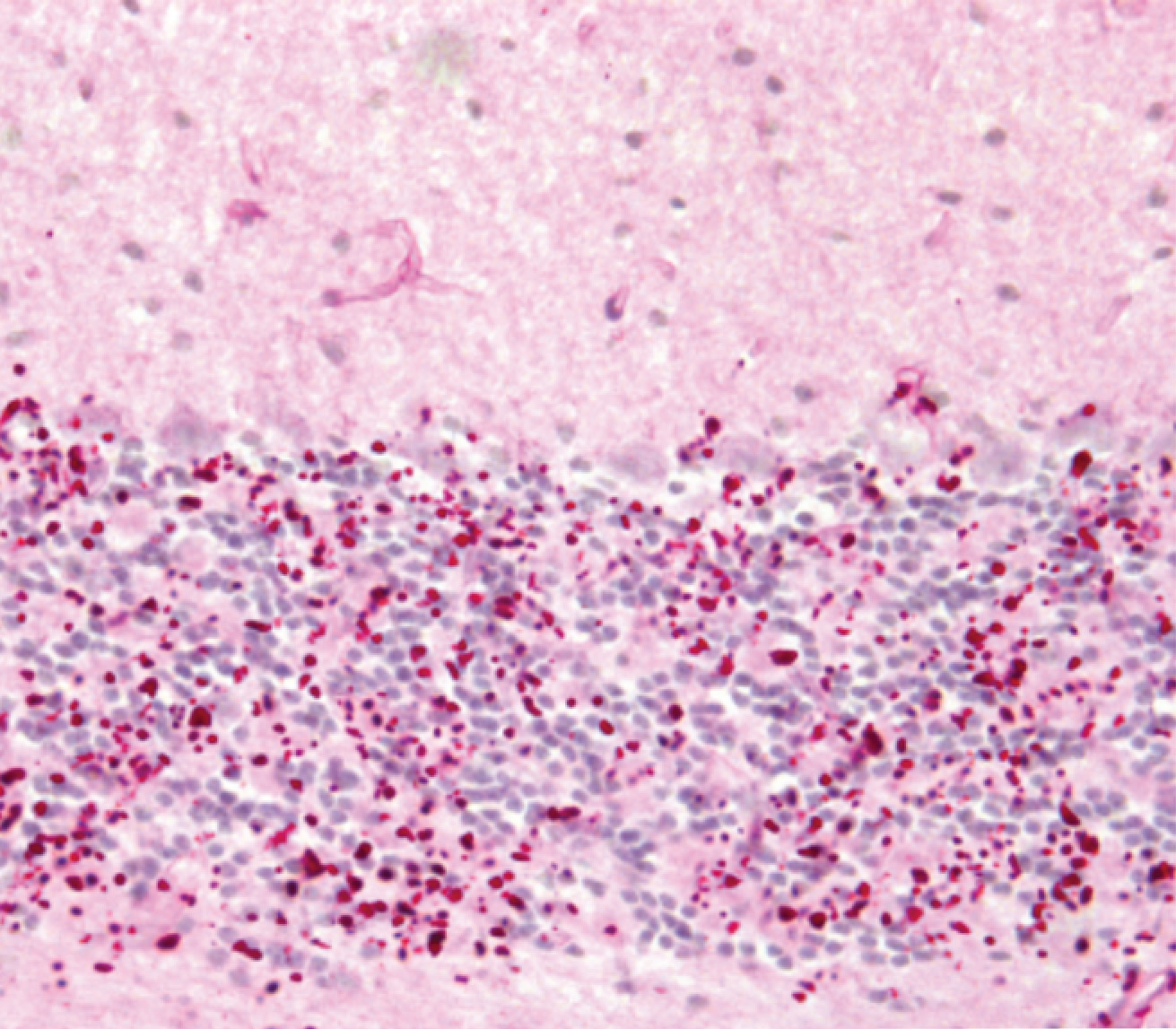
Lafora disease is a lethal disorder of adolescence, characterize by progressive myoclonus epilepsy and neurodegeneration, which is driven by its pathological hallmark, the Lafora body, first described over 100 years ago by the Spanish neurobiologist Gonzalo Rodríguez Lafora.
Based on the fact that one of the disease genes, laforin, encodes a glycogen phosphatase, and that glycogen in Lafora disease is hyperphosphorylated, a favored pathogenic mechanism for the last years has been that the basic defect leading to Lafora body formation is hyperphosphorylation of glycogen, which renders it insoluble.
These ideas were challenged by previous work published in 2014 in Brain by the group of Prof. Santiago Rodríguez de Córdoba at CIB. They reported that expressing phosphatase-inactive laforin in laforin-deficient mice eliminates the formation of lafora bodies and rescues the disease phenotype, concluding that the phosphatase function of laforin is dispensable.
The paper now published in EMBO Molecular Medicine in collaboration with Dr. Berge Minassian supports and extends the preceding conclusions. The experiments confirm that indeed, glycogen hyperphosphorylation is not damaging to glycogen and does not lead to Lafora body formation. Current data supports that Lafora bodies are formed as a result of local glycogen chain length pattern disturbance and that laforin cooperates with the ubiquitin E3 ligase malin to regulate glycogen chain length distribution.
Although future experiments are still needed to fully understand how the laforin-malin complexes act to prevent generation and/or accumulation of glycogen with abnormally elongated chains and prevent the formation of the lafora bodies, these two publications by Rodríguez de Cordoba’s laboratory represent a major landmark in the understanding of Lafora disease.
Reference: Abnormal glycogen chain length pattern, not hyperphosphorylation, is critical in Lafora disease. Nitschke F, Sullivan MA, Wang P, Zhao X, Chown EE, Perri AM, Israelian L, Juana-López L, Bovolenta P, Rodríguez de Córdoba S, Steup M, Minassian BA. EMBO Mol Med. pii: e201707608. doi: 10.15252/emmm.201707608. (2017).

