Hutchinson-Gilford Progeria Syndrome (HGPS) is an infrequent genetic condition that accelerates ageing. The most serious consequence of HGPS is the early onset of cardiovascular disease.
Now, a team from the Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC), the Centro de Investigaciones Biológicas Margarita Salas (CIB-CSIC) and the Instituto de Ciencias de Materiales de Madrid (ICMM-CSIC) has made a significant advance in understanding the underlying causes of cardiovascular disease in patients with HGPS. Specifically, they have identified the activation of the YAP/TAZ pathway in endothelial cells as a key factor in developing atherosclerosis in this disorder. This finding, published in The Journal of Clinical Investigation, offers new insights into the vascular problems affecting patients with HGPS and opens up new avenues for treatment.
HGPS is a rare genetic disorder caused by a mutation in the LMNA gene, which causes the synthesis of a toxic protein called progerin that accelerates cellular ageing. People with HGPS show signs of rapid ageing in early life and develop severe atherosclerosis in adolescence, leading to cardiovascular complications that usually result in premature death around the age of 14.5 years. Despite their severity, the mechanisms that cause cardiovascular problems in patients with HGPS have not been fully elucidated.
The team, led by Dr Andrés, head of the Molecular and Genetic Cardiovascular Pathophysiology group at the CNIC and principal investigator at the Centro de Investigación Biomédica en Red sobre enfermedades cardiovasculares (CIBERCV), and Dr Ignacio Benedicto, head of the Vascular Ageing group at the CIB-CSIC and visiting scientist at the CNIC, explored how the cells that line the blood vessels, known as endothelial cells, are affected in this disease.
They used advanced single-cell RNA sequencing technology to analyze the gene expression of the different cell types present in the arterial wall of HGPS mouse models and healthy control mice.
This approach allowed them to examine the transcriptional activity of individual cells in unprecedented detail.
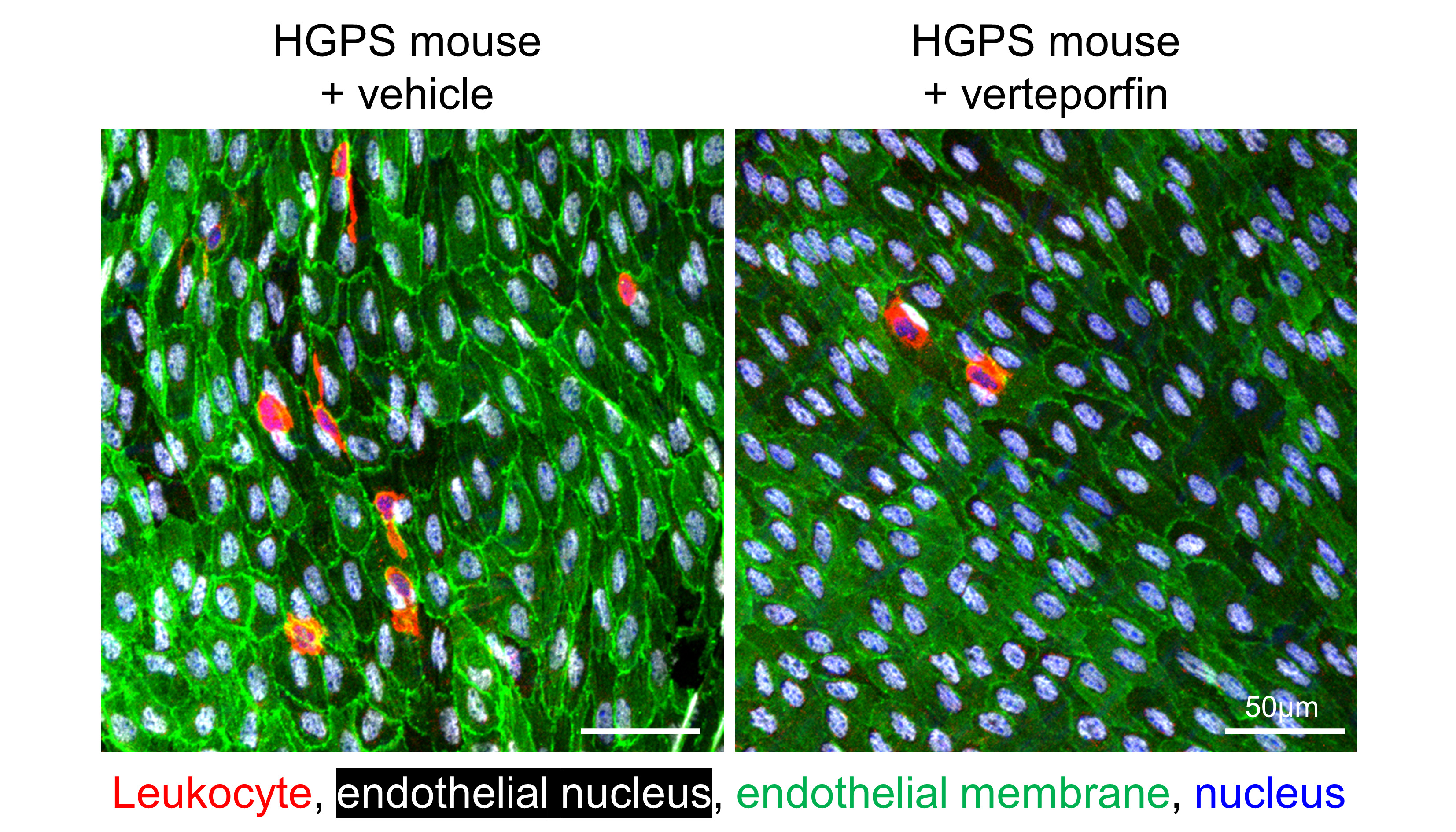
Their results revealed that endothelial cells in HGPS undergo significant changes in gene expression related to inflammation, immune cell recruitment and stiffening of the surrounding extracellular matrix. One of the most prominent findings was the activation of the YAP/TAZ signalling pathway, a critical regulator that allows cells to respond to mechanical forces, such as blood flow and stiffening of their environment. The researchers found that in HGPS mice, this pathway was abnormally active in endothelial cells in the aorta, the main artery that carries blood from the heart to the rest of the body.
‘Our findings suggest that hardening of the arterial wall and changes in blood flow patterns in HGPS patients activate the YAP/TAZ pathway in endothelial cells. This, in turn, promotes inflammation and the accumulation of immune cells in the arteries, which accelerates the development of atherosclerosis,’ explains Dr Ana Barettino, first author, of the research.
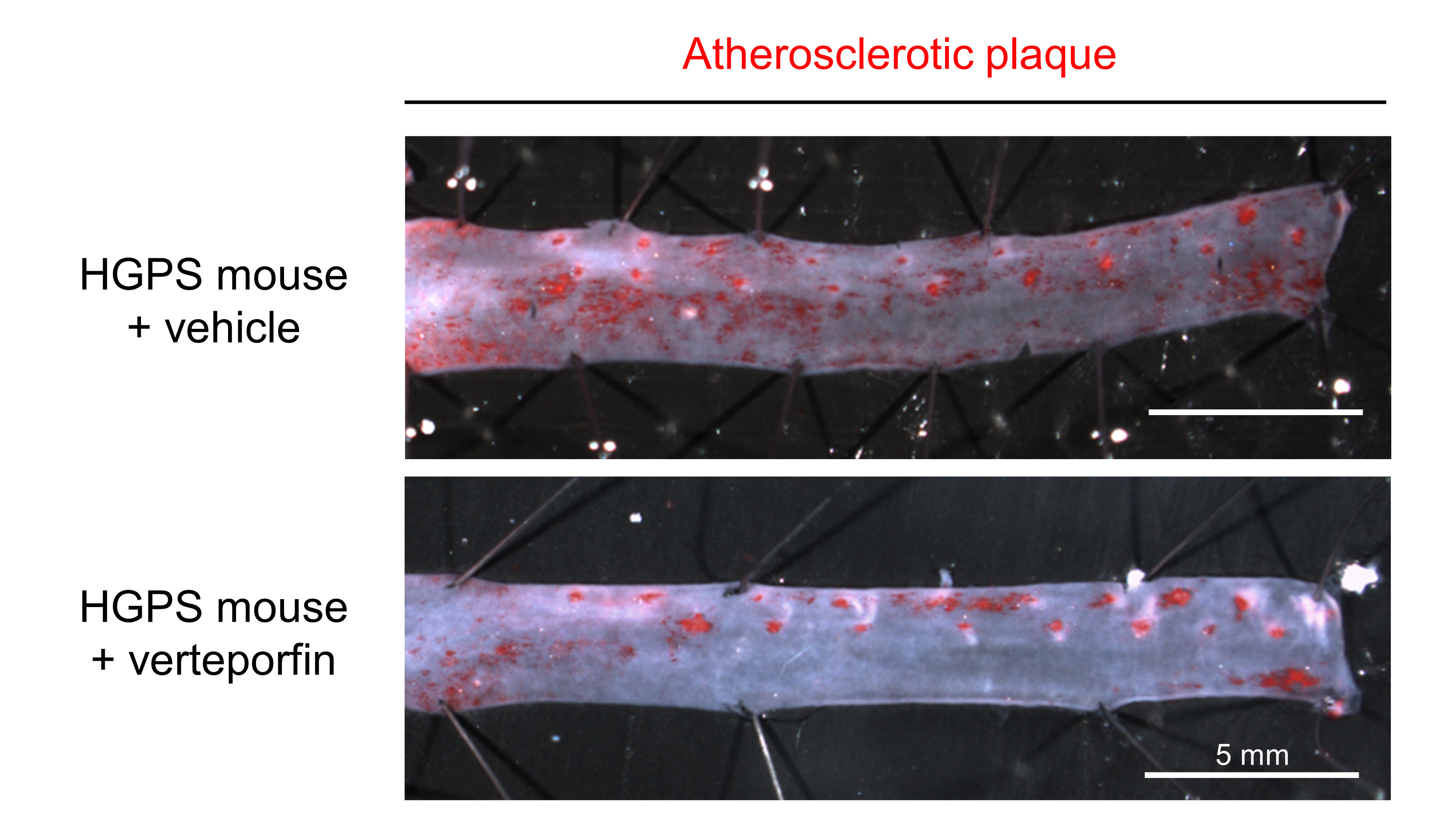
The team also explored the possible therapeutic implications of these findings. They tested whether inhibition of the YAP/TAZ pathway could reduce the progression of atherosclerosis in HGPS mice.
They used verteporfin, a drug already approved by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the treatment of age-related macular degeneration.
The results showed that treatment of HGPS mice with verteporfin significantly decreased the development of atherosclerosis, additionally reducing endothelial cell activation and immune cell accumulation in the aorta, two key factors in atherosclerosis.
‘The results in our mouse model are very encouraging, as by inhibiting the YAP/TAZ pathway we were able to significantly reduce the progression of atherosclerosis, the main medical problem in patients with HGP,’ says Dr Vicente Andrés.
However, they acknowledge that more work is needed to fully understand the role of the YAP/TAZ pathway and how it could be safely inhibited in patients with HGPS.
One potential concern is that the YAP/TAZ pathway is also involved in many normal biological processes, including tissue repair and regeneration. Therefore, any therapy aimed at inhibiting this pathway would need to be carefully designed to avoid unwanted side effects.
‘Our study represents an important step in understanding the mechanisms behind vascular ageing in HGPS,’ notes Dr Barettino. ‘However, translating these findings into a safe and effective treatment for patients will require further research. We need to investigate how we can specifically target therapy to inhibit the YAP/TAZ pathway in diseased cells without affecting healthy tissues.’
In addition to its relevance to HGPS, the study has wider implications for understanding cardiovascular disease in the general population.
Atherosclerosis is a leading cause of death worldwide, and many of the processes identified in this progeria study, such as vascular stiffening and activation of inflammatory pathways, are also present in arteries as we age.
‘The knowledge we have gained from studying HGPS may help us to better understand the ageing process in general and the factors that contribute to cardiovascular disease in older people,’ adds Dr Andrés.
In this sense, Dr Benedicto stresses that ‘by studying the molecular pathways that drive vascular ageing, we could develop new therapies that improve quality of life and promote healthy ageing’.
This study has been funded by grants from the Ministry of Science, Innovation and Universities (MICIU) and the State Research Agency (AEI) (MICIU/AEI/10. 13039/501100011033); FEDER/EU and ‘NextGenerationEU’/PRTR funds (PID2022-141211OB-I00, PID2022-137111OA-I00, RYC2021-033805-I), and Comunidad de Madrid with co-financing from IEE/ESF funds (2017-T1/BMD-5247, 2021-5A/BMD-20944).
Reference: Endothelial YAP/TAZ activation promotes atherosclerosis in a mouse model of Hutchinson-Gilford progeria syndrome. Barettino A, González-Gómez C, Gonzalo P, Andrés-Manzano MJ, Guerrero CR, Espinosa FM, Carmona RM, Blanco Y, Dorado B, Torroja C, Sánchez-Cabo F, Quintas A, Benguría A, Dopazo A, García R, Benedicto I*, Andrés V* (2024) J Clin Invest. Oct 1:e173448, doi: 10.1172/JCI173448

